|
Epigenetic Changes After Trauma May Be Adaptive, Contribute to Resilience
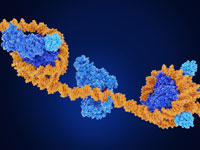 | |
In recent years, research throughout the scientific and medical community has suggested a link between trauma and epigenetic changes, chemical modifications that affect gene activity without actually changing the gene’s DNA sequence. The assumption has been that epigenetic changes in the context of trauma are inherently bad, a form of damage that gets passed from generation to generation. But according to Rachel Yehuda, Ph.D., Endowed Professor of Psychiatry and Neuroscience of Trauma at the Icahn School of Medicine at Mount Sinai, these changes may also be adaptations that promote resilience.
“Sometimes the biological changes in response to trauma or intergenerational trauma are there to help deal with the problem of trauma, not compound its effects,” Yehuda said. “The survival advantage of this form of intergenerational transmission depends in large part on the environment encountered by the offspring themselves.”
|